IRS Allows HDHPs to Pay for COVID-19 Testing, Treatment Pre-Deductible
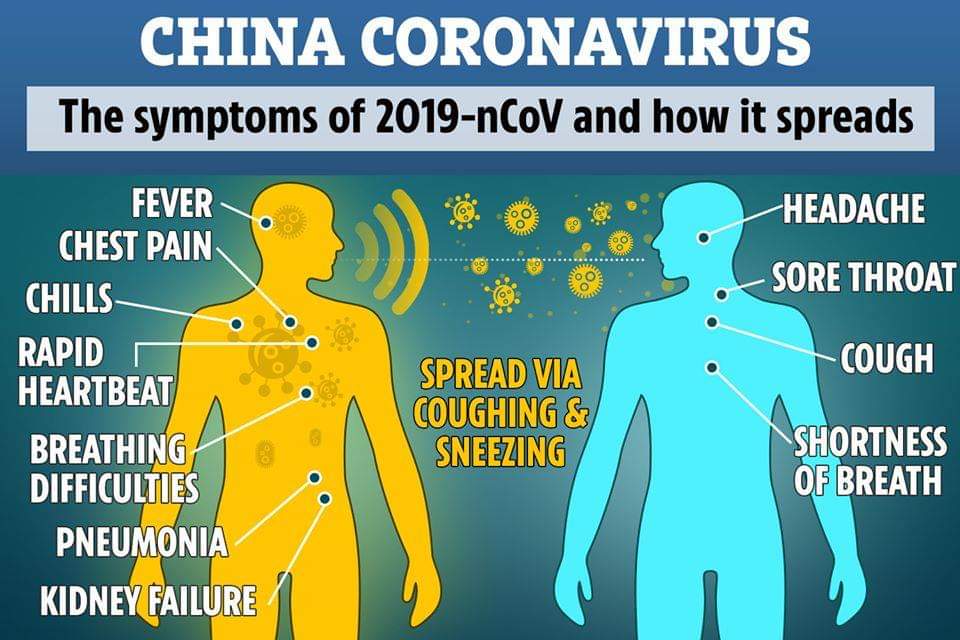
The IRS has issued new emergency guidance that allows insurers to waive the cost of coronavirus testing and treatment for individuals who are enrolled in high-deductible health plans (HDHPs). Major health insurers report they’ve been concerned that if they can make the change to their high-deductible plans without breaching IRS regulations regarding such plans. Specifically, […]
IRS Allows HDHPs to Pay for COVID-19 Testing, Treatment Pre-Deductible Read More »